Scrub Typhus
Scrub Typhus
- What is it?
- Why is it known as scrub typhus?
- What are the characteristics of the causative organism?
- How is the disease transmitted?
- Is the occurrence of scrub typhus outbreaks seasonal?
- Incubation period of scrub typhus
- Clinical symptoms of scrub typhus
- Diagnostic tests
- Treatment
- What precautions should be taken to protect you from scrub typhus?
- Related links
What is it?

Scrub typhus is an acute, febrile, infectious illness that is caused by Orientia (formerly Rickettsia) tsutsugamushi. It is also known as tsutsugamushi disease. Scrub typhus was first described from Japan in 1899. Humans are accidental hosts in this zoonotic disease.
Why is it known as scrub typhus?
The term scrub is used because of the type of vegetation (terrain between woods and clearings) that harbours the vector; however, the name is not entirely correct because certain endemic areas can also be sandy, semi-arid and mountain deserts.
What are the characteristics of the causative organism?
It is an obligate intracellular gram-negative bacterium that has a large number of serotypes. This pathogen does not have a vacuolar membrane; thus, it grows freely in the cytoplasm of infected cells. Because they are intracellular parasites, they can live only within the cells of other animals. Even though it is recognized as one of the tropical rickettsioses diseases, O. tsutsugamushi has a different cell wall structure and genetic composition than that of the rickettsiae. O. tsutsugamushi includes heterogeneous strains classified in five major serotypes: Boryon, Gilliam, Karp, Kato and Kawazaki. Differentiation of serotypes is important for laboratory diagnosis. Orientia tsutsugamushi can be cultivated on L929 cells and stained using the Giemsa method.
How is the disease transmitted?
Scrub typhus is transmitted to humans and rodents by some species of trombiculid mites (“chiggers”, Leptotrombidium deliense and others). The mite is very small (0.2 – 0.4mm) and can only be seen through a microscope or magnifying glass.
Humans acquire the disease from the bite of an infected chigger. The bite of the mite leaves a characteristic black eschar that is useful to the doctor for making the diagnosis.
The adult mites have a four-stage lifecycle: egg, larva, nymph and adult. The larva is the only stage (chigger) that can transmit the disease to humans and other vertebrates, since the other life stages (nymph and adult) do not feed on vertebrate animals. Both the nymph and the adult are free-living in the soil.
Is the occurrence of scrub typhus outbreaks seasonal?
Yes. The seasonal occurrence of scrub typhus varies with the climate in different countries. The period of epidemic is influenced by the activities of the infected mite. It occurs more frequently during the rainy season. However, outbreaks have been reported during the cooler season in southern India. Certain areas such as forest clearings, riverbanks, and grassy regions provide optimal conditions for the infected mites to thrive.
Incubation period of scrub typhus
The incubation period of scrub typhus is about 5 to 20 days (mean, 10-12 days) after the initial bite.
Clinical symptoms of scrub typhus
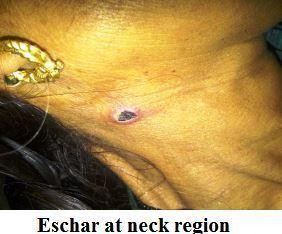
 The chigger bite is painless and may become noticed as a transient localized itch. Bites are often found on the groin, axillae, genetalia or neck. An eschar is often seen in humans at the site of the chigger bite. The illness begins rather suddenly with shaking chills, fever, severe headache, infection of the mucous membrane lining the eyes (the conjunctiva), and swelling of the lymph nodes. A spotted rash on the trunk may be present. Eschars are rare in patients in countries of South-East Asia and indigenous persons of typhus-endemic areas commonly have less severe illness, often without rash or eschar. Whether this is due to past exposure to the organism, or to other factors, is unknown. Symptoms may include muscle and gastrointestinal pains. More virulent strains of O. tsutsugamushi can cause haemorrhaging and intravascular coagulation. Complications may include atypical pneumonia, overwhelming pneumonia with adult respiratory distress syndrome (ARDS)–like presentation, myocarditis, and disseminated intravascular coagulation (DIC). Patients with scrub typhus often exhibit leucopenia.
The chigger bite is painless and may become noticed as a transient localized itch. Bites are often found on the groin, axillae, genetalia or neck. An eschar is often seen in humans at the site of the chigger bite. The illness begins rather suddenly with shaking chills, fever, severe headache, infection of the mucous membrane lining the eyes (the conjunctiva), and swelling of the lymph nodes. A spotted rash on the trunk may be present. Eschars are rare in patients in countries of South-East Asia and indigenous persons of typhus-endemic areas commonly have less severe illness, often without rash or eschar. Whether this is due to past exposure to the organism, or to other factors, is unknown. Symptoms may include muscle and gastrointestinal pains. More virulent strains of O. tsutsugamushi can cause haemorrhaging and intravascular coagulation. Complications may include atypical pneumonia, overwhelming pneumonia with adult respiratory distress syndrome (ARDS)–like presentation, myocarditis, and disseminated intravascular coagulation (DIC). Patients with scrub typhus often exhibit leucopenia.
Acute scrub typhus appears to improve viral loads in patients with HIV. This interaction is currently unexplained. Clinical scrub typhus is not known to occur naturally in animals.
Diagnostic tests
The diagnosis may be confirmed by a laboratory test such as serology. The cheapest and most easily available serological test is the Weil-Felix test, but this is notoriously unreliable. Fifty per cent of patients have a positive test result during the second week. This test is now being replaced by a complement-fixation test. It is a serological test to detect specific antibody or specific antigen in a patient’s serum. Each patient’s serum is systematically tested against five O. tsutsugamushi serotypes. An IgM titer > 1:32 and/or a four-fold increase of titers between two sera confirm a recent infection. However, due to cross-reactions among serotypes, it is difficult to identify accurately a specific serotype.
The gold standard is indirect immunofluorescence antibody (IFA). Indirect immunoperoxidase (IIP) is a modification of the standard IFA method that can be used with a light microscope, and the results of these tests are comparable to those from IFA. Serological methods are most reliable when a four-fold rise in antibody titre is looked for. Although many techniques have been used successfully for sero diagnosis, relatively few are used regularly by most laboratories.
Commercial rapid diagnostic kits provide reliable and well-accepted preliminary results within one hour, but the availability of these tests is severely limited by their cost. However, other serological tests must be used in order to obtain confirmationof O. tsutsugamushi infection. ELISA provides more sensitivity and equal specificity when compared to commercial test kits.
The organism can be grown in tissue culture or mice from the blood of patients with scrub typhus but results are not available in time to guide clinical management. Molecular detection using polymerase chain reaction (PCR) is possible from skin rash biopsies, lymph node biopsies or ethylenediaminetetraacetic acid (EDTA) blood. O. tsutsugamushi can be demonstrated by standard and by nested PCR. Real time PCR assays are as sensitive as standard PCR but are more rapid and can give quantitative results .
Treatment
There is paucity of evidence based on randomized controlled trials for the management of O. tsutsugamushi diseases including scrub typhus. These guidelines for treatment cover the most common infection, the scrub typhus, murine typhus and Indian Tick typhus and do not cover acute Q fever though treatment of Q fever is on similar lines. Without waiting for laboratory confirmation of the O. tsutsugamushi infection, antibiotic therapy should be instituted when O. tsutsugamushi disease is suspected.
At Primary level
The Health Care provider needs to do the following
- Recognition of disease severity - If the patients come with complications to primary health facility and treating physician considers it as O. tsutsugamushi infection, treatment with doxycycline should be initiated before referring the patient.
- Referral to secondary or tertiary centre in case of complications like ARDS, acute renal failure, meningo-encephalitis, multi-organ dysfunction. In addition to recommended management of community acquired pneumonia, doxycycline is to be initiated when scrub typhus is considered likely.
- In fever cases of duration of 5 days or more where malaria, dengue and typhoid have been ruled out; following drugs should be administered when scrub typhus is considered likely –
Adults
- Doxycycline 200 mg/day in two divided doses for individuals above 45 kg for duration of 7 days. Patients should be advised to swallow capsules with plenty of fluid during meals while sitting or standing Or
- Azithromycin 500 mg in a single oral dose for 5 days.
Children
- Doxycycline in the dose of 4.5 mg/kg body weight/day in two divided doses for children below 45 kg
- Azithromycin in the single dose of 10mg/kg body weight for 5 days.
Pregnant women
- Azithromycin 500 mg in a single dose for 5 days.
- Azithromycin is the drug of choice in pregnant women, as doxycycline is contraindicated
At secondary and tertiary care
- The treatment as specified above in uncomplicated cases.
- In complicated cases the following treatment is to be initiated –
- Intravenous doxycycline (wherever available) 100mg twice daily in 100 ml normal saline to be administered as infusion over half an hour initially followed by oral therapy to complete 7-15 days of therapy. OR
- Intravenous Azithromycin in the dose of 500mg IV in 250 ml normal saline over 1 hour once daily for 1-2 days followed by oral therapy to complete 5 days of therapy. OR
- Intravenous chloramphenicol 50-100 mg/kg/d 6 hourly doses to be administered as infusion over 1 hour initially followed by oral therapy to complete 7-15 days of therapy.
- Management of the individual complications should be done as per the existing practices. Doxycycline and/or Chloramphenicol resistant strains have been seen in South-East Asia. These strains are sensitive to Azithromycin.
What precautions should be taken to protect you from scrub typhus?
- In endemic areas, precautions include wearing protective clothing.
- Insect repellents containing dibutyl phthalate, benzyl benzoate, diethyl toluamide, and other substances can be applied to the skin and clothing to prevent chigger bites.
- Do not sit or lie on bare ground or grass; use a suitable ground sheet or other ground cover.
- Clearing of vegetation and chemical treatment of the soil may help to break up the cycle of transmission from chiggers to humans to other chiggers.
Related links
- Guidelines for Diagnosis and Management of Rickettsial Diseases in India
- Communicable Disease Alert on Scrub Typhus and other Rickettsioses
Source: World Health Organization
Last Modified : 7/3/2023
This topic covers about Breast Cancer causes, symp...
This topic provides information related to the com...
This topic discuss about Acute Lymphocytic Leukemi...
This topic discuss about risk factors, symptoms, d...
