Contraception for Adolescents
Contraception for Adolescents
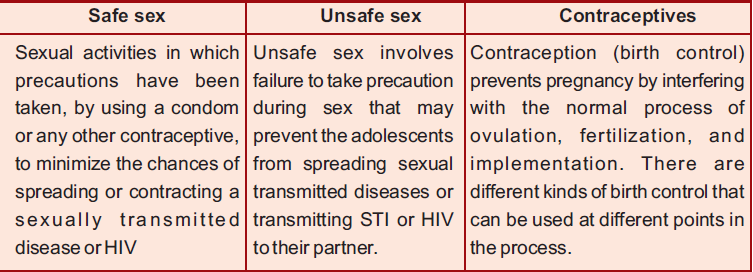
Definition of Contraception
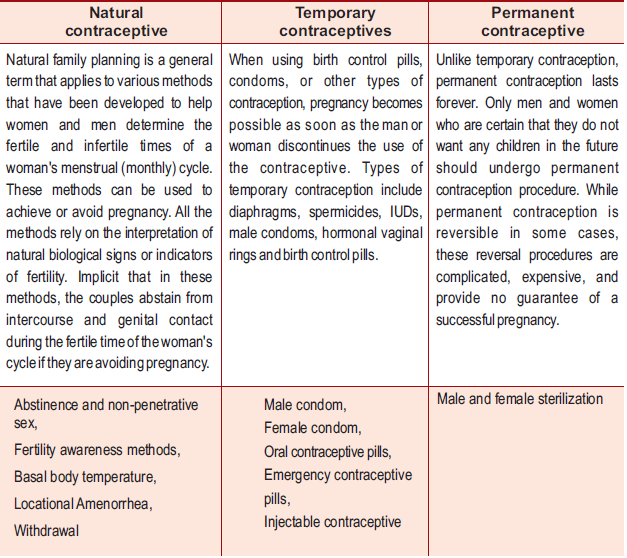
Contraception (birth control) prevents pregnancy by interfering with the normal process of ovulation, fertilization, and implementation.There are different kinds of birth control that can be used at different points in the process.
Why Adolescents need Contraceptive Methods
Most adolescents begin their sexual activity without adequate knowledge about sexuality or contraception or protection against STIs/HIV. In India, though adolescent marriages are very common in rural areas, the couple is less likely to use contraception than adults. Most women who marry young have the first child early.
For unmarried adolescents it is sometimes impossible to access contraceptives and the sexual activity often results in unintended pregnancy.
Whether married or unmarried, adolescents face potentially serious physical, psychological and social consequences from unprotected sexual relations, ranging from early and unwanted pregnancy and childbirth, unsafe abortion to STIs including HIV/AIDS. The consequences can also be far reaching and affect their entire life chances and options, especially in the case of girls.
Barriers to contraceptive use among adolescents
The barriers that adolescents face in accessing contraceptives are:
- The unexpected and unplanned nature of sexual activity
- Lack of information and knowledge about conception and contraceptives and their availability.
- Fear of medical procedures
- Fear of judgemental attitudes of providers
- Inability to pay for services and transport
- Fear of opposition from partner or parents
- Pressure to have children.
Care providers are unaware and insensitive to the special needs of adolescents. They needs to overcome their attitudes and moral and tradition-related biases and respond to the special needs of adolescents by designing and reorienting health services to meet those needs.
Health care providers need to also be aware of gender inequalities that alienate and marginalize adolescent girls in their communities and prevent them from seeking technically skilled care.
Need for providing Adolescents with Information and Education on Sexuality and contraception
In a country like ours where tradition and societal norms are very rigid, education on sexuality and reproductive health for adolescents has not spread beyond a handful of enlightened schools and individuals because of concerns that such knowledge would lead to promiscuity. On the contrary, failure to provide adolescents with appropriate and timely information represents a missed opportunity for reducing the incidence of unwanted pregnancy and STIs and their negative consequences.
Sexual and reproductive health education needs to be formalized and tailored to suit the needs of adolescents who have not begun sexual activity, and those who are already sexually active. Research into the sexual and reproductive health of young people clearly points to the fact that information provision and education alone do not necessarily lead to behaviour change. Increasing awareness and understanding is only the first step in preventing unwanted pregnancy and STI/ HIV. Also, adolescents must know where to locate such services.
Health workers should involve important members of the community such as school teachers, influential elderly ladies and men, local pharmacist, youth leader to help promote information and education on sexuality and contraception during any informal contact they have with adolescents or their parents. For this you can hold meetings with these “gate keepers” to sensitise them to contraceptive needs of the adolescents.
Providing Adolescents with Contraceptive Services
Health care providers can act as change-agents within the families and communities by advocating need of contraceptive services, thus preventing the consequences of too early and unprotected sexual activity among adolescents.
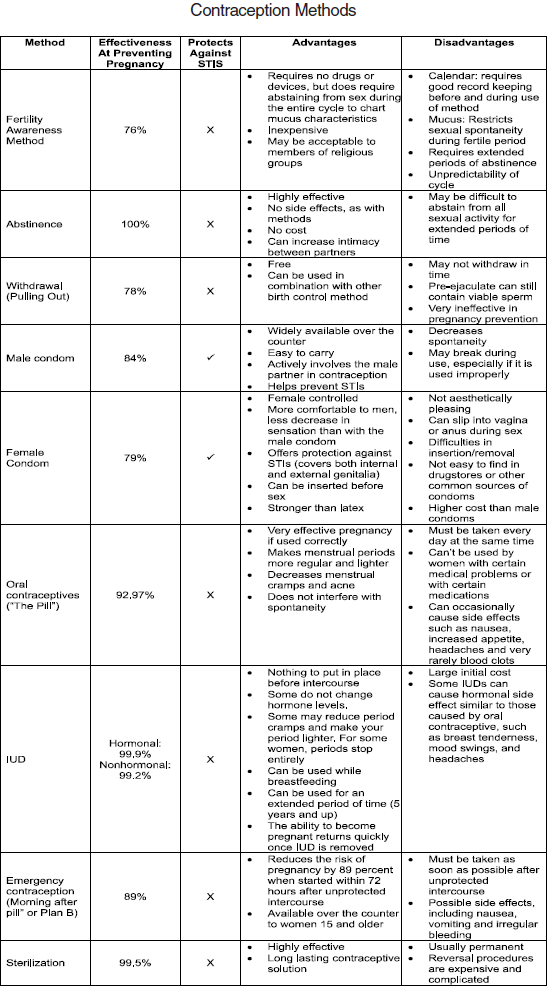
The following Table lists the effectiveness of the available contraceptive methods in preventing pregnancy and in providing protection from STIs/HIV.
Emergency Contraception
Progestin only OCPs containing the hormone levonergstrel can be used for emergency contraception. If the correct dose is started within 72 hours after unprotected intercourse, it reduces the chances of pregnancy. Now oral contraceptives are being packaged as emergency contraceptive pills, and levonorgestrel - only tablets are more effective and cause less nausea and vomiting. Emergency contraception has a special role for adolescent girls and women who are subjected to sexual violence, to prevent unwanted pregnancies. There is a need to increase access to ECPs by training healthcare providers and also by ensuring easy availability of ECPs. All adolescents are eligible for ECP, without restriction on repetitive use.
Contraceptive Methods
Counselling
Adolescence is a critical period in an individual’s life when at the threshold of adulthood, they experiment with new behaviours, and struggle with issues of independence, and peer group pressure.
The first step towards counseling adolescents is to develop a rapport with them and also speak in a language they understand. A supportive and non-judgemental environment, where confidentiality is ensured, is essential but is easier said than done. Health-care providers need special training in sexuality counselling skills so that they can deal with the needs, concerns and problems of adolescents. They also need to overcome their own barriers about sexual behaviour, morality, etc.
The special needs adolescents may have include bodily changes, information regarding ‘Normal and abnormal’ feelings and actions. Service providers who are not comfortable discussing these issues with adolescents, should refer them to those who are.
Counselling should cover responsible sexual behaviour and needs to be directed at both males and females. Male adolescents should be encouraged to share the responsibility for contraception and STI/HIV prevention with their female partners.
While adolescents may choose to use any contraceptive method available to them, some may be more appropriate for a variety of social and behavioural reasons. Many of the needs and concerns of adolescents that affect their choice of a contraceptive method are similar to those of adults seeking contraception. For example, using a method that does not require a daily regimen, such as oral contraceptive pills do, may be a more appropriate choice for an individual.
In helping an adolescent make a choice of which method to use, health- care providers must provide them with information about the methods, and help them consider their merits and demerits. In this way, they could guide their adolescent clients to make well-informed and voluntary choices of the method that is most suitable to their needs and circumstances (taking eligibility, practicality and legality into consideration).
The information provided should address the following issues:
- Effectiveness of the method
- Information on protection against STIs/HIV
- Common side-effects of the method
- Potential health risks and benefits of the method
- Information on return to fertility after discontinuing use of the method
- Where the method can be obtained and how much it costs.
After a method is chosen, it is also important to discuss correct use of the method and follow-up information, such as signs and symptoms that would necessitate a return to the clinic.
It is important to remember that even if married, adolescents may have other special information needs. They may be particularly concerned about their return to fertility after discontinuing use of a method. Most women would be under considerable pressure to have children, and thus may want to keep their contraceptive use private from their spouse or in-laws.
Unmarried adolescents will be less likely to seek contraceptive services at health facilities because of the need for secrecy and fears that the staff may be hostile or judgemental. For those who do seek contraceptive services, it is important to discuss abstinence or non-penetrative sexual activity as options, even with those who have already had sexual intercourse. With support, individuals can delay sexual activity until they are older, and thus be better able to deal with its social, psychological and physical implications. This requires commitment, high motivation, self-control and negotiation skills. For the unmarried, condoms alone or in combination with another method - are the best recommendation and are easily available.
Adolescents who are coerced into having sex
Adolescents who have been subjected to sexual coercion and abuse will require special care and support. Emergency contraception is part of a package of services that should be made available in such circumstances. Health-care providers need to be sensitive to these issues. They must also be well aware of how to access the health and social services that these adolescents may need.
Sources :
Last Modified : 7/1/2024
This topic explains factors and variuos methods of...
e-Counselling is a one stop solution provides end-...
