Mental Health of Adolescents
Mental Health of Adolescents
- Introduction
- Mental Health and Adolescents
- Common mental and behavioural disorders seen in adolescents
- Risk and Protective factors for mental health of children and adolescents
- Consequences of adolescent mental illness
- Presentation and assessment of adolescent mental illnesses and substance abuse
- Attitudes towards adolescent mental health and stigma
- Responding to adolescents with mental illnesses or substance abuse
- Promoting mental health in adolescents
Introduction
Mental health is defined as a state of successful performance of mental function, resulting in productive activities, fulfilling relationships with other people, and the ability to adapt to change and cope with adversity. (US Surgeon General Report, Dec 1999)
Mental illness is a spectrum ranging from less serious to more serious conditions. Physical health can affect mental health, and vice versa.
The spectrum of mental health
The spectrum of mental health ranges from mental wellbeing to diagnosable mental and behavioural disorders that meet specified clinical criteria.
Mental well-being is a state in which the individual can realize his or her potential, cope with the everyday stresses of life, study or work productively, and participate in community life.
The positive dimension of mental health is stressed in the World Health Organization (WHO) constitution, where health is defined as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”. Mental well-being is therefore more than the absence of mental illness and cannot be achieved simply by preventing and treating mental disorders. It is also necessary to promote mental well-being by carrying out activities, providing services and creating environments that promote mental health.
Mental difficulties or problems are ways of thinking, feeling or behaving that impact negatively on an adolescent’s quality of life and development.
Mental difficulties or problems can be part of normal adolescent development; may be responses to events in the adolescent’s life or stressors. Mental difficulties or problems do not meet diagnostic criteria of disorders – they have a different duration, severity and impact.
Perceptions of what is “normal” or “abnormal” are determined to a large extent by the social and cultural context. Different ways of thinking and behaving across cultures may influence the way that mental illness manifests and is perceived.
Mental illness manifests through thoughts, feelings and behaviours of an individual.
- Thinking/thoughts (cognition): e.g. interpreting the words or actions of people as being against oneself.
- Feelings (emotion): e.g. experiencing certain emotions, such as sadness, fear or anger.
- Behaviours (action): e.g. withdrawing from or being aggressive towards others.
Mental Health and Adolescents
Mental health is strongly related to other health problems in adolescence, including substance abuse, violence, and sexual and reproductive health.
Common mental and behavioural disorders seen in adolescents
People who are diagnosed in adulthood with a mental disorder often experience their first episode of the disorder during adolescence. Many of the most serious disorders, such as schizophrenia, bipolar disorder and depression, are identified during the late adolescence or the beginning of adulthood). The pre-existing mental health problems may get worse as the adolescent undergoes this demanding phase of emotional and physical development.
The following are the more common mental and behavioural disorders of adolescence:
Anxiety disorders
Anxiety describes unpleasant feelings of apprehension, tension, fear or worry. These feelings can be associated with physical (bodily, somatic) symptoms, such as a fast heart rate, sweating or shaking. In adolescence, there may also be an effect on development.
Obsessive-compulsive disorder (OCD) is an anxiety disorder characterized by intrusive thoughts (obsessions) that produce uneasiness, apprehension, fear, or worry; by repetitive behaviours (compulsions) aimed at reducing the associated anxiety; or by a combination of such obsessions and compulsions.
Depression
Depression is a common mental disorder during adolescence. It is primarily characterized by sadness (feelings), loss of interest in activities (thoughts, behaviours) and decreased energy (physical symptoms). Other physical symptoms include difficulty concentrating and changes in appetite and sleep.
Sometimes, the physical symptoms are more obvious than the feeling of sadness. It is not uncommon for depression and anxiety to occur together in a mixed anxiety-depressive disorder.
Schizophrenia
Schizophrenia is a mental disorder where there is disturbed thinking and perception and often inappropriate emotions. Disturbed thinking can be recognized in the form of delusions – beliefs about people or things that remain fixed, despite evidence to the contrary; these are often bizarre or paranoid (e.g. the individual may believe the parents trying to kill him). Disturbed perception can be recognized in the form of hallucinations – sensory perception of something or someone that is not present (e.g. hearing voices that speak about the individual in the third person). Behaviours are also affected and may seem strange to an observer.
Substance use disorders
There are a number of disorders resulting from the abuse of psychoactive substances such as alcohol, opioids (heroin), cannabinoids (marijuana), sedatives and hypnotics, cocaine, other stimulants, hallucinogens, tobacco and volatile solvents. The conditions include acute intoxication, harmful use, dependence and psychotic disorders.
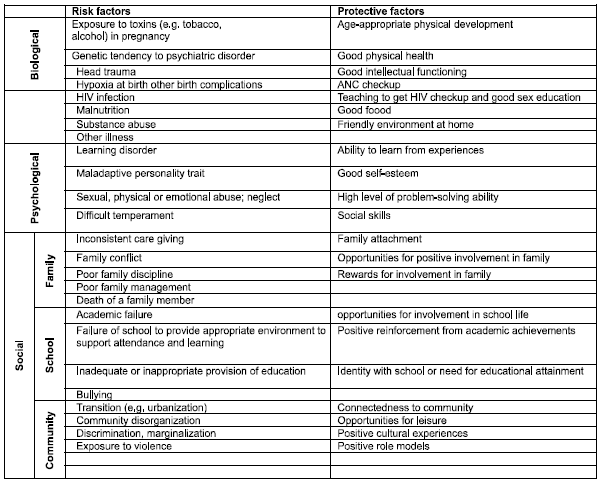
Risk and Protective factors for mental health of children and adolescents
Consequences of adolescent mental illness
Consequences of adolescent mental illness include:
- Suffering (e.g. personal distress, family distress);
- Functional impairment (e.g. inability to study, work, raise a family or be independent);
- Exposure to stigma and discrimination (e.g. isolation, missed opportunities, abuse from others);
- Increased risk-taking behaviour (e.g. unprotected sex, excessive alcohol use);
- Premature death (e.g. violence, suicide, overdose of drugs).
Some people think that a diagnosis of a mental health problem or a mental disorder implies that the person is doomed to have the problem for the rest of their life. Mental health problems, like physical illnesses, can be short- lived as well. A person diagnosed with mental health problems will not necessarily have the problem for the rest of his or her life.
Presentation and assessment of adolescent mental illnesses and substance abuse
Mental illness presenting through thoughts, feelings and behaviours
As discussed before, mental illnesses are expressed in thoughts, feelings and behaviours. Here are some examples of how we get information to assess an adolescent’s mental health when they come to the clinic:
- What the adolescent says about his or her thoughts and feelings;
- What the adolescent says he or she does (self-reported behaviour);
- Observing how the adolescent looks (self care) and speech (tone of voice);
- What other people (e.g. parents, teachers, other adults, siblings, peers) say the adolescent does or says about his or her thoughts and feelings;
- Observing the adolescent’s interactions with other people – behaviour;
- General physical examination;
- Medical records.
In addition to mental illness being evident through a person’s thoughts, feelings and behaviours, mental illness may also manifest as physical (bodily or somatic) symptoms. e.g.:
- Sleep problems or unexplained tiredness;
- Anxiety and palpitations;
- Dizziness, trembling and sweating;
- Generalized aches and pains (including of the head, chest and abdomen);
- Poor appetite or loss of weight.
Other presentations that might indicate underlying adolescent mental illness
There are also other presentations that should alert the health-care provider to possible mental health problems or a need for a mental health assessment, e.g.:
- Social withdrawal or reduced participation (in school, work or social activities);
- Declining academic performance;
- Signs of excessive and frequent alcohol or psychoactive substance use;
- Self-report or report by others of frequently engaging in high-risk behaviour (e.g. reckless driving, playing with firearms).
Changes in mood and behaviour can provide important indicators of an adolescent’s mental wellbeing, but these observations alone cannot be conclusive of mental illness – they can only indicate the need to carry out a full assessment.
It is important for health-care providers to be aware of these presentations, as they may point to underlying mental health problems.
The HEADS framework or approach can help the health-care providers assess whether an adolescent is mentally well or ill and, if they are ill, to assess the severity of the illness. The letters of HEADS remind the health-care provider of the issues that need to be discussed with the adolescent:
HEADS framework
H Home
E Education/employment;Eating; Exercise
A Activities
D Drugs;
S Sexuality; Safety; Suicide and depression.
It is necessary to discuss the HEADS approach in more depth, considering possible warning signs that might point towards adolescent mental illness.
Home
The home environment is an essential part of the adolescent’s life and hence a good area to begin the interview. This will help the health-care provider understand the family situation, e.g. whether the adolescent is living with parents (one or both) or a guardian.
Warning signs include the following:- Adolescent has no support at home or anywhere else.
Education/employment
The educational or work environment and the peer group in this setting are important factors in determining the mental health and well-being of adolescents and in influencing their behaviour.
Warning signs include the following:
- Adolescent is having trouble at school or work, e.g. problems with school or work, bullying, or problems with teachers or bosses.
- Adolescent frequently misses school or work.
Eating
The health-care provider should enquire about the adolescent’s body image and eating habits. An open-ended question could be “What do you think about your weight?” This opening can lead to questions on the adolescent’s eating habits, e.g. “Warning signs include the following:
- Adolescent is overweight and has poor eating habits.
- Adolescent believes he or she is overweight, when it is evident that this is not the case.
- Adolescent is absorbed or obsessive about food, exercise, body weight or shape.
- Adolescent is underweight, and from the discussion it appears that financial constraints are contributing to this.
Exercise
The health-care provider should ask the adolescent about their regular exercise routine. Warning signs include the following:
- Adolescent participates in no or very little physical activity.
- Adolescent is overweight and unfit (e.g. breathless, tires easily walking upstairs).
- Adolescent is absorbed or obsessive about exercise and body weight.
- Adolescent is undernourished or engages in excessive physical labour.
Activities
Asking the adolescent about what they enjoy doing for fun can give a picture of their behaviour
Warning signs include the following:- Adolescent has no friends and spends most of the time alone.
- Adolescent spends most of the time with people who are 4–5 years older, who affect his behaviours negatively.
Drugs
The health-care provider should routinely ask all adolescents some general questions about substance use.
Warning signs include the following:- Adolescent regularly uses legal or illegal substances.
- Adolescent has tried illegal substances or has friends who do so.
- Substance use is having a negative impact on adolescent’s health or ability to function.
- Other people have expressed concern about adolescent’s substance use.
Sexuality
This part of the interview requires care, as the information being obtained is sensitive. Discussions on sexuality need to take account of the social and cultural context of the adolescent. Concerns about sexual development, sexuality and sexual abuse are all sensitive topics and need to be approached in a careful and supportive manner with more focus on confidentiality
Warning signs include the following:- Adolescent is being or has been pressured to have sex.
- Adolescent seems at risk for early sexual activity.
- Adolescent has had unsafe sex or has had a number of sexual partners.
- Adolescent seems upset or worried about his or her sexual orientation.
Safety
The health-care provider should ask about safety issues at home, work and school, including questions regarding bullying and violence. Warning signs include the following:
- Adolescent is experiencing bullying, violence, sexual harassment or abuse.
- Adolescent is withdrawn and unable to talk of experiences, or examination reveals signs of violence.
Suicide and depression
Asking the adolescent about their mood and signs and symptoms of depression is important..
Warning signs include the following:- Adolescent is sad or anxious or feels hopeless most of the time.
- Adolescent talks about hurting or killing himself, or has tried to hurt or kill himself.
- Adolescent frequently uses alcohol or drugs to escape negative feelings.
- Adolescent has poor self-esteem and no sense of self-worth.
Attitudes towards adolescent mental health and stigma
The stigma of mental illness
Stigma is a mark of shame, disgrace or disapproval that results in an individual being shunned or rejected by others. In most societies, mental and behavioural disorders are associated with stigma, and this stigma tends to increase as behaviours become increasingly different from the “norm”.
Mental illness might be believed to be associated with evil spirits and magic.
Stigma can prevent people from acknowledging their own mental health problems and from disclosing them to others. Many people do not seek help when they need it for fear of being labelled as “mentally ill”.
They can result in- Rejection by friends, fellow students, co-workers, relatives and neighbours, leading to aggravated feelings of rejection, loneliness and depression;
- Rejection of the young person, which can affect his or her family or caregivers and lead to their isolation or humiliation;
- Denial of equal participation in family life, schooling, social and professional networks, and employment;
- Educed ability to access the services, treatment and support required in health-care settings and the community.
Health-care providers should be aware that adolescents with mental illness are more vulnerable to being abused and badly treated.
Reducing the stigma of mental illness for adolescents
The stigma of mental illness can be reduced by actions at the community and wider societal level. At the community level, there is a need to:
- Talk openly about mental illness and the role of the community in promoting mental health and supporting adolescents with mental illness;
- Provide accurate information on the causes, prevalence, course and effects of mental illness;
- Challenge the negative stereotypes and misconceptions surrounding mental illness, and challenge and correct myths and misinformation on the causes and treatment of mental illness, including among health workers;
- Provide support and treatment services that enable young people with mental illness to participate fully in all aspects of community life.
At the societal level, there is a need to:
- Ensure that those in charge of law and policy reform understand the issues surrounding adolescent mental health, and that they work towards the provision of mental health services in the community;
- Create demand and support for new or revised legislation and its enforcement to protect the rights of people with mental illness, enable access to health and social services, and reduce discrimination in schools and the workplace.
Myths, misconceptions and negative stereotypes about mental illness are a major cause of the stigma associated with mental illness. Therefore, reducing the stigma of mental illness involves talking openly and accurately about the causes, effects and effective treatment of mental illness. One example of this is to make people aware that most adolescent mental health problems are not permanent and can be treated successfully with bio-psychosocial interventions.
Features of Substance use/abuse in adolescents
Some of the most common symptoms of drug abuse in teenagers include lying, stealing, making repeated excuses (ie for asking for money, going out, going to bath-room) staying in their room, becoming verbally or physically abusive toward others, having items in their possession that are connected to drug use, the smell of drugs on them, mood swings, sleepless nights, changes in friends and academic decline. In addition to these more behavioral symptoms, look for the physical symptoms of drug intoxication and withdrawal.
Responding to adolescents with mental illnesses or substance abuse
Adolescents with mental health problems need to be identified in their communities and referred to primary-level health facilities where they should get the care and support they need. Adolescents requiring specialized care need to be referred to referral-level health facilities.
Responding to adolescents with mental health problems at the family and community level
Family members, teachers, youth workers, social workers and other non- health workers could help identify (in their homes, schools and elsewhere in their communities) adolescents experiencing mental health problems. To do this, they need to know what warning signs to be alert to. They also need to know that it is important to look out for these warning signs.
They could also help adolescents experiencing mental health problems by giving them a patient hearing, empathizing and offering advice and support to adolescents to cope with the challenges they are facing and to deal with them effectively. If the symptoms persist or if the adolescent’s ability to function is affected, he or she should be referred to a primary-level health- care facility. Family and community members can make it easier for adolescents to seek help by normalizing and legitimizing care-seeking for mental health problems.
Responding to adolescents with mental health problems at the primary level
Supporting the substance abuser medically is the approach to managing most drug antoxication/withdrawals, sure many substances of abuse can affect bodily functions (for eg. heart rate, blood pressure, breathing rate) In addition to medical management, psycheatric assessment is also required, sence drugs are associated with impaired judgement, secure aggression, assaultive behaviour and ever judicidal homicidal behaviors.
Pasychosocial interventions & pharmacotherapy play a vital role in the management of drug dependance and to prevent relapse. Help from mental health professionals & other trained health care professionals makers should be sought the psychosocial intermantions involve the adolescent his/her parents & others concerned persons. The pharmacoceutical agents are used as delerrants or anti crausing agents or healthier and less harmful replacement agents.Promoting mental health in adolescents
Many sectors have complementary contributions to make to crafting an effective overall response to promoting mental health in adolescents, preventing problems from arising, and responding to mental health problems promptly, effectively and sensitively. For this to happen, ministries of health need to:
- Engage and support other sectors - in particular, the education, social welfare, media, employment, youth and sports sectors - to make important contributions;
- Ensure their actions are evidence-based, are carried out well, reach all adolescents (especially those who are most vulnerable), and are carried out collaboratively with other sectors.
The term “life skills” refers to a generic set of skills that can be learnt at any stage in life for the promotion of psychosocial competence among young people and that can be applied to many areas of life. The table below gives some examples of life skills.
| Setting | Sector | Actions |
|---|---|---|
| Home | Social welfare services |
Educating parents to help them understand the emotional needs of adolescents and how to respond to these needs Nature of mental health problems that might occur,how to respond to them,and when and how to seek help Supporting vulnerable adolescents and their families |
| School | School Staff |
Building individual assets such as self-esteem and life skills Discussing sexual health, injuries, violence and substance use; promoting healthy attitudes and behaviours Making school a safe (i.e.free from physical and emotional violence) and supportive (i.e, where students and staff feel valued and supported) environment Training teachers to detect adolescents who might need help, provide them with counselling support, and refer those who need medical help to health facilities Working with social health services to identify and provide support to adolescents living in difficult circumstances |
| Community | Community leaders and members |
Engaging and sensitizing community leaders and members to create a caring and supportive environment for adolescents with or at risk of mental health problems,and their families Engaging and senstizing community members to intervene when there is violence in homes and elsewhere in the community Training selected community members to detect and refer to health services adolescents who might need help |
| Media and Communication Technology | Media Personnel |
Disseminating information on factors contributing to mental health problems in adolescents, on effective ways to prevent mental health problems and respond to them when they occur, and on substance use and mental health problems Preventing glamorization of suicide |
| Communication and interpersonal skills | Decision-making and critical thinking skills | Coping and self-management skils |
|---|---|---|
|
Interpersonal communication skills: Verbal/non-verbal communication Active listening Expressing feelings, giving feedback (without blaming), receiving feedback |
Decision-making and Information-gathering Skills: Evaluating future consequences of actions or self and others Determining alternative solutions to problems Analysis skills regarding influence of values and attitudes about self and others on motivation |
Skills for increasing personal confidence and abilities to assume control, take responsibility, make a difference or bring about change: Building self-esteem and confidence Creating self-awareness skills, e.g.awareness of rights, influences, values, attitudes, strengths, weaknesses Setting goals Self-evaluation, self assessment, self-monitoring |
|
Negotiation/refusal skills: Negotiation and conflict management Assertiveness Refusal Empathy building Ability to listen, understand another's needs and circumstances, and express that understanding Cooperation and teamwork: Expressing respect for others contributions and different styles Assessing own abilities and contributing to the group |
Critical thinking skills: Analysing peer and media influences Analysing attitudes, values, social norms, beliefs, and factors affecting them Identifying relevant information and sources of information |
Skills for managing feelings: Managing anger Dealing with grief and anxiety Coping with loss, abuse and trauma
Skills for managing stress: Time management Positive thinking Relaxation techniques |
|
Advocacy Skills: Influencing skills, persuasion Networking, motivation |
Source : Rashtriya Kishor Swasthya Karyakram - Resource Book by Ministry of Health and Family Welfare
Last Modified : 7/1/2024
This topic provides information about Sim Card Swa...
This topic deals with information related to Anxie...
The Article provides information about Antioxidant...
This topic deals with information related to Appen...
